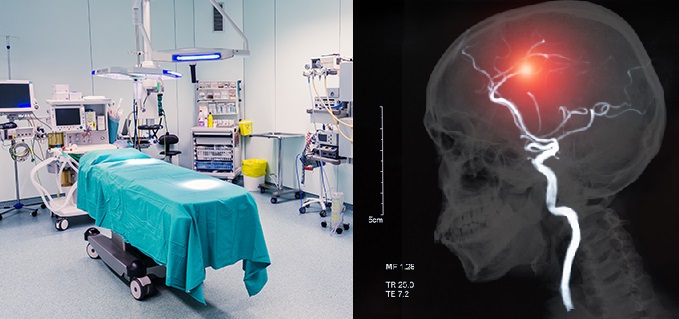
Perioperative Management of Stroke Patient
Perioperative Stroke
Perioperative strokes result in prolonged hospital stays, disability, and death.
Most perioperative strokes are embolic or ischemic; hemorrhagic strokes are rare.
In healthy patients undergoing non-cardiovascular surgery, the stroke risk is extremely small (0.04–0.8%); In contrast, patients with a history of CVA or TIA are at increased risk of perioperative stroke.
In the largest series in the literature, 173 patients with a prior stroke underwent general anesthesia, and recurrent stroke occurred in 2.9% (5 of 173).
Perioperative Stroke Risk Factors
In estimating the overall risk of perioperative stroke, a number of other risk factors have been identified. Prominent among these is atrial fibrillation, which is present in approximately one third of perioperative strokes.
Additional risk factors that should be considered are advanced age, hypertension, smoking, and prior neurologic symptoms.
The types of procedures with the highest incidence are cardiac, carotid, and aortoiliac surgery with rates of perioperative stroke in the range of 1% to 5%.
Timing of Surgery After Stroke
Elective surgery should probably be postponed for at least 1 month after an ischemic stroke.
In the absence of definitive evidence, many experts currently recommend that general surgery should be avoided within 2 to 3 weeks of an acute stroke if possible, and elective surgery should be delayed for 2 to 3 months.
Preoperative Evaluation
In most cases, patients with few risk factors for perioperative stroke undergoing low-risk noncardiac surgery do not need further testing.
In patients with stroke history and planned cardiac procedure, including aortic manipulation, performing a transesophageal echocardiography to identify aortic atherosclerotic plaques should be considered.
A frequently encountered scenario is the preoperative assessment of patients with suspected carotid stenosis undergoing major surgery.
The decision should be individualized on a patient-by-patient basis.
Patients with a history of stroke or TIA should be screened with Doppler ultrasound, or magnetic resonance imaging (MRI) or computed tomography (CT) angiography, if previous evaluation has not been done or if the patient’s neurological status has worsened since the stroke.
In patients in whom an asymptomatic high-grade stenosis is detected before undergoing a major cardiovascular surgery, consider brain imaging with CT or MRI to exclude clinically silent ipsilateral territorial infarcts and intracranial MRA or CTA, or transcranial Doppler to determine the hemodynamic significance of the area of stenosis and the status of intracranial blood flow.
Patients in whom carotid stenosis is judged to be symptomatic or hemodynamically significant may require preoperative carotid revascularization to minimize their perioperative stroke risk.
Management of Antithrombotic Drugs
Abrupt discontinuation of antiplatelet agents before surgery may be associated with increased risk for stroke recurrence due to rebound hypercoagulability.
Aspirin should be stopped only 2 to 3 days before major neurosurgical procedures.
Continuation of aspirin therapy is acceptable during regional spinal anesthesia, nerve blocks, dermatological cutaneous surgeries, dental procedures, ophthalmological procedures, peripheral vascular procedures, cardiac surgeries, and endoscopies.
Clopidogrel, on the other hand, appears unsafe and should be discontinued 5 to 7 days before surgical Procedures.
There are no studies regarding the safety of dipyridamole, alone or in combination with aspirin, during surgery. It is therefore prudent to withhold it 5 to 7 days preoperatively.
A good practice may be substituting clopidogrel and dipyridamole with aspirin in patients at high risk for stroke during the preoperative period.
For many patients taking warfarin for stroke prevention, the risk of perioperative discontinuation of anticoagulation exceeds the risk of bleeding complications. Preoperative bridging therapy with heparin is advised and warfarin is discontinued. Heparin can be stopped hours prior to the procedure and warfarin restarted 24 hours after surgery.

1 Comment
Normand Lysher
18 October, 2020
I¡¦ve recently started a website, the info you offer on this site has helped me greatly. Thank you for all of your time & work.
https://forex-scams.com/top-10-best-online-brokers/