Brain Metastasis, A Practical Approach
Brain Metastasis, An Overview
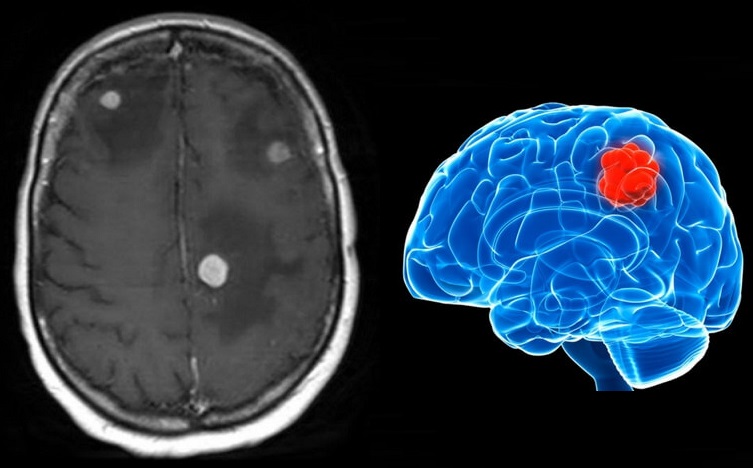
Parenchymal brain metastasis is the most common direct neurological complication of systemic cancer.
Brain metastases can arise anywhere in the brain, and their frequency in various locations reflects the relative proportion of cerebral blood flow. Thus 80% of metastases arise in the supratentorial compartment.
For unclear reasons, pelvic and gastrointestinal primary tumors are more likely to metastasize to the posterior fossa than to the supratentorial region.
Brain metastases are the initial manifestation of an underlying primary tumor in 10% to 30% of cases.
Lung cancer is the most common cause of brain metastases presenting without a known primary, accounting for two-thirds of cases.
Among lung tumor metastases, two-thirds are from non–small cell lung cancer (NSCLC).
Their precise incidence is unknown, but they outnumber primary tumors by a 10 : 1 ratio.
Current estimates range from 20% to 40% of those dying with cancer.
Overall, lung cancer accounts for 40% to 50% of all patients with brain metastases, and breast cancer accounts for 15% to 20%. Melanoma, renal cell carcinoma, and gastrointestinal tumors each account for an additional 5% to 10% of cases.
The overall incidence of brain metastases appears to be rising.
One possible explanation is improved survival of systemic disease, allowing more time for development of brain metastases. Additionally, the blood-brain barrier prevents systemic chemotherapeutic agents from treating brain metastases.
Clinical Features
Symptoms of brain metastases may arise as long as 20 years after discovery of the primary tumor, or may even antedate discovery of the underlying systemic cancer.
The latter is common with lung cancer, whereas patients with systemic breast cancer and melanoma may enjoy years of apparent freedom from systemic cancer prior to discovery of cerebral Metastasis.
The presenting features are usually progressive over days to weeks, although occasional patients present acutely with seizures or stroke-like syndrome in the setting of intratumoral hemorrhage.
Patients who present clinically with brain metastases can have signs of increased intracranial pressure (headache, nausea, and vomiting), mental status changes, seizures, or focal signs.
Leptomeningeal carcinomatosis can present similarly, except that focal signs are more often exhibited by cranial nerve abnormalities and can have a multifocal distribution indicating the widespread process.
Seizures are present at diagnosis in 18% of patients with brain metastases.
Mental status changes and hemiparesis are the most common findings on neurological examination.
Despite the frequent occurrence of increased intracranial pressure, papilledema is detectable in only 10% of patients.
Differential Diagnosis
See the complete list of clinical and radiological differential diagnosis of cerebral metastasis in “NeuroAdvise” application. See the home page for more information: https://www.neuroadvise.com/
Brain Metastasis, A Practical Approach
When neurological symptoms and/or signs develop in a patient with known systemic cancer, brain metastasis must always be suspected.
Diagnosis also may be suspected based on imaging studies.
Careful medical history and physical examination with emphasis on the presence/activity of the systemic disease and the general physical condition (estimation of the performance status) are recommended.
There has been significant controversy regarding how much initial diagnostic evaluation is needed for patients with cancer from an unknown primary site.
The goals of evaluation should be to identify patients with favorable clinical and histopathologic features for whom specific treatment is available.
For example, specific treatment is available for patients with lymphoma and metastatic cancer arising from the thyroid gland, breast and prostate, and other reproductive organs.
A thorough review of systems is a key component to the initial diagnostic evaluation and not only helps to locate the primary site of most symptomatic brain metastases but also to ascertain the general functional status of the patient, which is critical before making further treatment decisions.
In many cases, the history reveals organ-specific complaints that guide further diagnostic work-up, including a comprehensive physical examination, screening laboratory studies, and limited imaging evaluation.
The physical examination evaluates all lymph node basins in the groin, axilla, head, and neck and includes palpation of the thyroid gland, digital rectal examination, and careful skin examination.
This basic physical assessment should also include breast and gynecologic examinations in women and prostate and testicular examinations in men.
The essential laboratory work-up should include a complete blood count, electrolyte panel, calcium concentration, liver function tests, amylase, lipase, stool for occult blood, and urinalysis.
Tumor markers that are detectable in serum include prostate-specific antigen (PSA), cancer-associated antigen 125 (CA-125), and carcinoembryonic antigen (CEA); these markers may be nonspecifically increased in patients with cancer but generally lack sufficient sensitivity or specificity as screening tools.
serum PSA may be useful in men with brain metastases and diffuse metastatic disease to bone or lungs.
In general, tumor markers are more valuable for following the effects of treatment than for making a specific diagnosis.
In the absence of organ-specific signs or symptoms, the initial radiographic work-up should include a chest x-ray and computed tomography (CT) scans of the chest, abdomen, and pelvis.
Chest CT may disclose lung masses not shown by chest radiography.
Although use of mammography rarely detects an occult primary site in women with brain metastases, the implications for treatment may justify its use in women, because effective treatment for breast cancer does exist.
The finding of a lung mass must be interpreted cautiously, because many other tumor types that metastasize to the brain do so by first metastasizing to the lungs.

3 Comments
ปั้มไลค์
26 June, 2020
Like!! Thank you for publishing this awesome article.
spinal
30 September, 2020
Very good article! We will be linking to this great post on our site. Keep up the great writing.
https://www.sendspace.com/file/0ug8j2
Eusebio Hazarika
18 October, 2020
There is visibly a bundle to realize about this. I suppose you made various nice points in features also.
https://forex-scams.com/top-10-forex-brokers-for-beginners/