Coma, Overview of Anatomic Localization
Coma and related states, definitions
Consciousness: state of awareness of self and environment
Alertness: An alert patient is fully conscious and aware of their environment
Confusion: inability to think with customary speed, clarity, and coherence.
Lethargy: difficult to maintain the arousal state
Obtundation: responsive to stimulation other than pain
Stupor: responsive only to pain
Coma: the patient is unconscious, unaware, and unresponsive to external stimuli
Delirium: clouding of consciousness with reduced ability to sustain attention to environmental stimuli.
Encephalopathy: a broad term used to denominate a syndrome of diffuse cerebral dysfunction
Some of the above terms are not rigidly defined and it is useful to record both stimulus and response
Neuroanatomy of consciousness
Maintaining alertness is primarily a function of the ascending reticular activating system (ARAS), which projects from the brainstem tegmentum through synaptic relays in the rostral intralaminar and thalamic nuclei to the cerebral cortex
Awareness is primarily a function of the cortex, with contributions from the precuneus and anterior cingulate gyrus
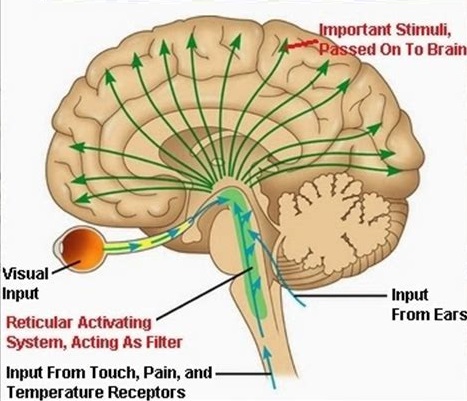
Figure 1: Anatomy of consciousness
Coma, overall approach to the patient
Several different states of impaired cognition or consciousness may appear similar to coma or be confused with it
Differentiation of these states from true coma is important to allow administration of appropriate therapy and help determine prognosis.
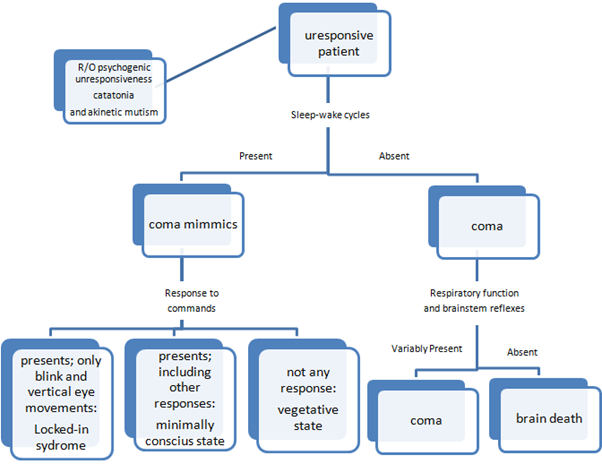
Algorithm 1: Approach to unresponsive patient
Then the patient should be classified into one of the following groups:
1. Coma with FNDs
2. Coma with meningismus
3. Coma without FND or meningismus
History & systemic examination
1. After the patient becomes stable, take history from accompanies
a. Determine the course
b. Similar events that happened before
c. Medical and social history
d. Drug history and substance abuse
e. Symptoms before onset of coma
2. Important systemic examination: vital signs, meningeal irritation, general appearance, Examination of skin, nails, mucosal membranes, respiration (including odor), heart and lung auscultation
Neurologic examination
1. The purpose is to differentiate structural from nonstructural causes and then to localize structural causes within neuraxis
2. Consists of four major parts:
a. Respiratory pattern
b. Pupils
c. Ocular movements
d. Motor response
Respiratory pattern
A, Cheyne-Stokes respiration: diffuse forebrain damage, upper brainstem damage, metabolic encephalopathy, impending transtentorial herniation
B, Central neurogenic hyperventilation: lesions of rostral brainstem (hyperventilation is more common in metabolic acidosis, pulmonary congestion, hepatic encephalopathy and analgesic overdosage)
C, Apneusis: pontine lesions specially infarct, rarely with metabolic coma or transtentorial herniation
D, Cluster breathing: lower pontine tegmental lesion
E, Ataxic breathing: lesion of the reticular formation of the dorsomedial part of the medulla.
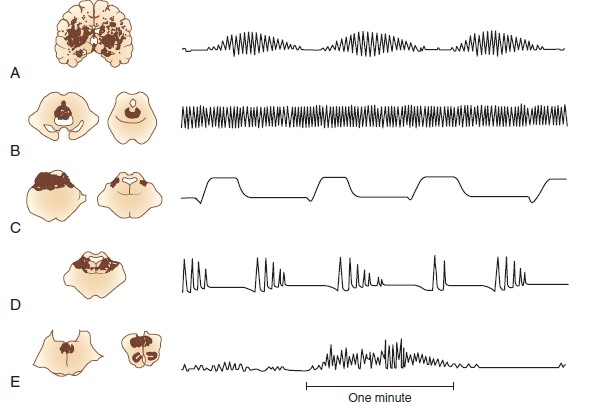
Figure 2: Respiratory patterns in comatose patient
Pupils
Anisocoria is always considered pathologic in comatose patient and represents an abnormality in autonomic innervation.
3rd nerve compression: dilated fixed
Sympathetic system damage (hypothalamus, medulla, cervical ganglion,…): Horner’s syndrome
Thalamus: small reactive
Midbrain: midposition, fixed
Pons: pinpoint reactive
Metabolic diseases: usually small reactive, (dilated unreactive pupils after anoxic coma suggests a bad prognosis)
Metabolic diseases do not affect pupil reactivity (except for anticholinergic and barbiturate poisoning and hypotherima)
Opiate poisoning causes small reactive pupils
Unilateral or bilateral mydriasis can be seen during or soon after epileptic seizures.
Ocular movements
1. Conjugate deviation:
a. To the side of hemiparesis: destructive cerebral lesion
b. To the opposite side of hemiparesis: pontine lesion, adversive seizure, thalamic hemorrhage
c. Downward: thalamic or midbrain lesion, metabolic (barbiturate poisoning)
d. Ping-pong gaze: bilateral cerebral infarct or cerebellar ICH
e. Bobbing: pontine, cerebellar, metabolic
2. Disconjugacy: paresis of specific EOMs, INO, unmasked preexisting phoria or tropia, skew deviation (cerebellar or pontine lesion)
3. Nystagmus
4. Oculocephalic and oculovestibular testing
Motor response
1. Spontaneous movements: myoclonus, clonic jerking, automatism
2. Muscles tone (hypotonia, hypertonia, paratonia)
3. Simple motor commands
4. Response to noxious stimuli
5. Posturing: Decorticate and decerebrate (often with hemispheric lesions or metabolic coma)
Flexor response implies more rostral lesion and better prognosis.
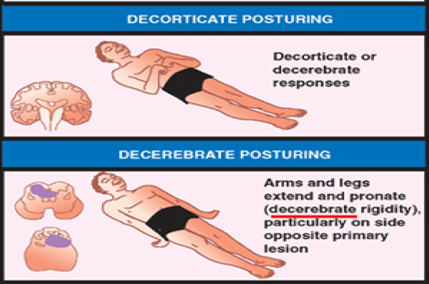
Figure 3: Motor response
Differentiating Toxic-Metabolic Coma from Structural Coma
1. The time course: structural lesions have a more abrupt onset, whereas metabolic or toxic causes are more slowly progressive
2. Multifocal structural diseases such as vasculitis or leukoencephalopathy are an exception to this rule, as they may exhibit slow progression
3. Response to initial emergency therapy
4. Structural lesions have focal features or at least notable asymmetry on neurological examination. Toxic, metabolic, and psychiatric diseases are characterized by their symmetry
5. Any toxic-metabolic cause of coma may be associated with focal features; however, such features most often are observed with barbiturate or lead poisoning, hypoglycemia, hepatic encephalopathy, and hyponatremia. Old structural lesions with residual abnormalities and unmasking of subclinical underlying disease may be the cause of focal signs
6. Structural lesions that may mimic toxic-metabolic causes include: SAH, CVT, chronic or bilateral subdural hemorrhage, and other diffuse or multifocal disorders such as vasculitis, demyelinating diseases, or meningitis
7. State of consciousness. Patients with metabolic problems often have milder alterations in arousal, typically with waxing and waning of the behavioral state. Patients with acute structural lesions tend to stay at the same level of arousal or progressively deteriorate. Toxins may also cause progressive decline in level of arousal.
8. Respiration. Deep, frequent respiration most commonly is due to metabolic abnormalities, though rarely it is caused by pontine lesions or by neurogenic pulmonary edema secondary to acute structural lesions.
9. Funduscopic examination. Subhyaloid hemorrhage or papilledema are almost pathognomonic of structural lesions. Papilledema due to increased ICP may be indicative of an intracranial mass lesion or hypertensive encephalopathy. Papilledema does not occur in metabolic diseases except hypoparathyroidism, lead intoxication, and malignant hypertension.
10. Pupil size. The pupils usually are symmetrical in coma from toxic-metabolic causes. Patients with metabolic or toxic encephalopathies often have small pupils with preserved reactivity.
11. Exceptions occur with methyl alcohol poisoning, which may produce dilated and unreactive pupils, or late in the course of toxic or metabolic coma if hypoxia or other permanent brain damage has occurred
12. Pupil reactivity. Assessment of the pupillary reflex is one of the most useful means of differentiating metabolic from structural causes of coma. Pupillary reactivity is relatively resistant to metabolic insult and usually is spared in coma from drug intoxication or metabolic causes, even when other brainstem reflexes are absent. Hypothermia may fix pupils, as does severe barbiturate intoxication. Neuromuscular blocking agents produce midposition or small pupils, and glutethimide and atropine dilate them.
13. Ocular motility. Asymmetry in oculomotor function typically is a feature of structural lesions
14. Spontaneous eye movements. Roving eye movements with full excursion are most often indicative of metabolic or toxic abnormalities
15. Reflex eye movements. Reflex eye movements normally are intact in toxic-metabolic coma, except rarely in phenobarbital or phenytoin intoxication or deep metabolic coma from other causes.
16. Adventitious movement. Periods of motor restlessness, tremors, or spasm punctuating coma often are due to drugs or toxins such as chlorpromazine or lithium. Brainstem herniation or intermittent CNS ischemia also may produce unusual posturing movements. Myoclonic jerking generally is metabolic and often anoxic in origin
17. Muscle tone. Muscle tone usually is symmetrical and normal or decreased in metabolic coma. Structural lesions cause asymmetrical muscle tone. Tone may be increased, normal, or decreased by structural lesions
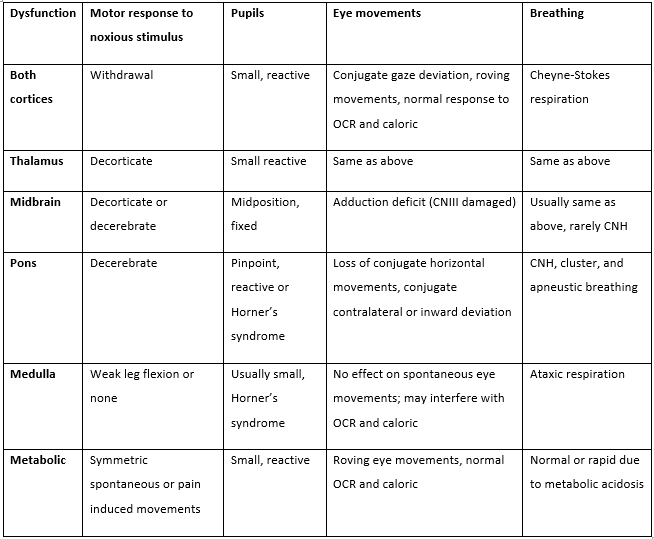
Table 1: Coma, overview of lesion localization
Brain herniation
Clinical features:
1. Increased ICP is always present.
2. A history of headache before the onset of coma, vomiting, severe hypertension beyond the patient’s static level, unexplained bradycardia, and subhyaloid retinal hemorrhages (Terson syndrome) are immediate clues to the presence of increased intracranial pressure, usually from one of the types of cerebral hemorrhage.
3. Papilledema develops within 12 to 24 h in cases of brain trauma and hemorrhage.
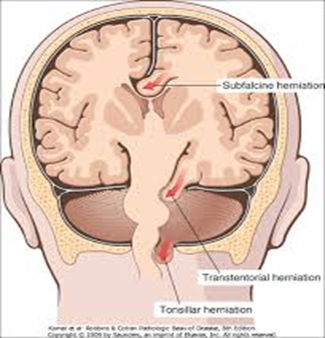
Figure 4: Syndromes of brain herniation
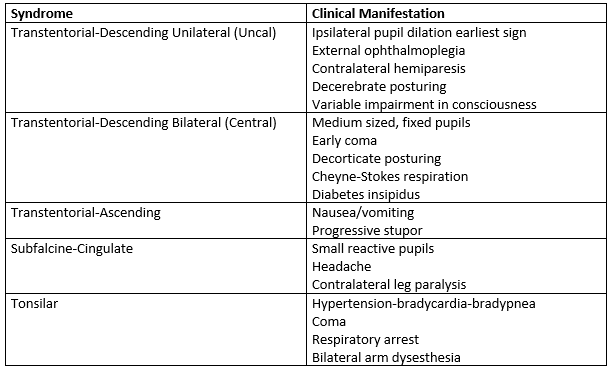
Table 2: Clinical features of herniation syndromes


2 Comments
YourFriendPablo
19 February, 2019
Great, I really like it! Youre awesome
Logan Pashal
16 October, 2020
I simply couldn’t go away your website prior to suggesting that I actually loved the standard information a person supply to your guests? Is going to be back frequently in order to check out new posts
https://forex-scams.com/top-10-fx-trading-brokers-in-the-world/