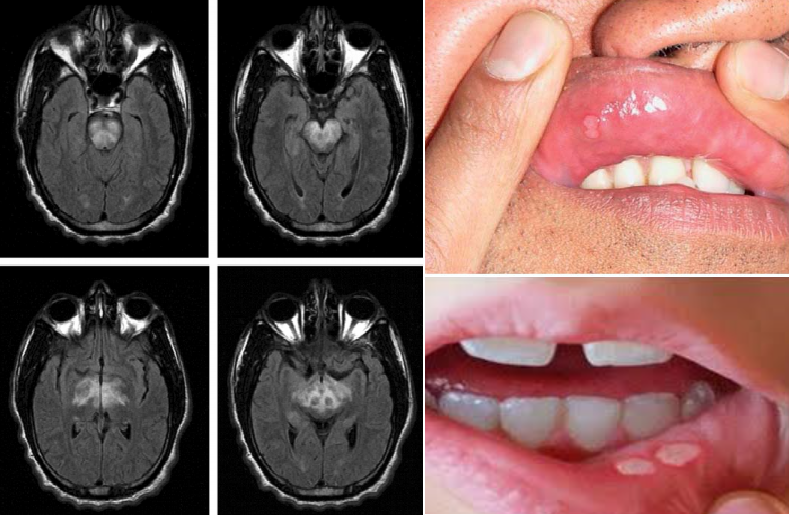
Behcet syndrome in a young man, presented with acute brainstem dysfunction
Behcet syndrome is a chronic, multisystem vasculitis that has no predilection to the type or size of vessel.
Neurologic involvement occurs in about one in five patients.
Epidemiology of Behcet syndrome
Behcet syndrome is most common in the Middle East and Eastern Asia with prevalence ranges from 13.5 to 35 per 100,000. In North American and Northern European countries, the prevalence is from 1 to 7 per 100,000.
There is no gender predilection; the disease typically affects young adults 20 to 40 years of age.
Clinical Manifestations of Behcet syndrome
Behcet syndrome is characterized by uveitis and recurrent oral and genital aphthous ulcers. Other manifestations include ocular, cutaneous, joint, gastrointestinal, or CNS inflammatory lesions. Small vessel vasculitis, thromboangiitis, vessel thrombosis, arteritis, and arterial aneurysms may occur.
CNS involvement is present in 20% of patients and can be subdivided into parenchymal (inflammation of the CNS tissue) or nonparenchymal (vascular neuro-behcet).
Parenchymal disease may be due to lesions in the corticospinal tract, periventricular white matter, basal ganglia, brain stem, and spinal cord. Clinical presentations are often subacute and manifestations may include headache, behavior changes, encephalopathy, acute meningeal syndromes, hemiparesis, hemisensory loss, seizures, cranial neuropathies, cerebellar dysfunction, alterations in mental status, and optic neuropathy. Spinal cord lesions may occur in isolation. Vascular manifestations may include diffuse vasculitis, venous sinus thrombosis, and uncommonly stroke due to arterial thrombosis, dissection, or aneurysm. In contrast to other systemic vasculitides, peripheral neuropathy is not commonly seen in Behcet syndrome.
Diagnosis of Behcet syndrome
Due to the lack of a specific diagnostic laboratory test, the diagnosis is made based on clinical criteria. The Behcet International Study Group (ISG) criteria and the International Criteria for Behcet’s Disease (ICBD) both require the presence of recurrent oral ulcers in addition to a constellation of recurrent genital ulcers, eye lesions (anterior or posterior uveitis or retinal vasculitis), or skin lesions (including erythema nodosum, pseudovasculitis, papulopustular lesions, or acneiform nodules consistent with Behcet). The ICBD also adds the presence of vascular lesions (superficial phlebitis, deep vein thrombosis, arterial thrombosis, or aneurysm formation) to the diagnostic criteria. Nonspecific markers of inflammation such as proinflammatory cytokines, circulating immune complexes, CSR, and the ESR may be elevated.
Treatment of Behcet syndrome
Treatment is dependent on the severity of the disease and the organ systems involved. Glucocorticoids or other immunosuppressive agents should be considered for treatment of erythema nodosum and pyoderma gangrenosum. Posterior uveitis and neurologic involvement require prompt treatment with both high-dose glucocorticoids and a second immunosuppressive agent (azathioprine, tumor necrosis factor [TNF]-alpha inhibitors, cyclosporine, interferon α, cyclophosphamide, and methotrexate).
Differential diagnosis of acute brainstem disorder (by NeuroAdvise system):
1. Inflammatory/autoimmune disorders: Multiple sclerosis; Behcet's disease; Wegener's granulomatosis; Polyarteritis nodosa; Churg-Strauss syndrome; Balo's concentric sclerosis; Bickerstaff's brainstem encephalitis; Marburg disease; Takayasu arteritis; Primary angiitis of the central nervous system; Sarcoidosis; Microscopic polyangiitis; Acute disseminated encephalomyelitis; Systemic lupus erythematous; 2. Acquired metabolic disorders: Osmotic myelinolysis; Hypoglycemia; Beriberi; Wernicke encephalopathy; 3. Cerebrovascular disorders: Brainstem infarction; Hypoxic-ischemic encephalopathy; Cerebral venous sinus thrombosis; Brainstem hemorrhage; Intracranial arteriovenous malformation; Subclavian steal syndrome; Vertebrobasilar dissection; 4. Primary/idiopathic disorders: Basilar migraine; 5. Non-neoplastic compressive disorders:Cavernous angioma; Central herniation; Uncal herniation; 6. Neoplastic disorders: Intracranial metastasis (e. g. from Lung cancer, Melanoma, Renal cell carcinoma, Colorectal cancer, Lymphoma); Brainstem glioma ; 7. Infectious disorders: Atypical bacterial brainstem encephalitis (Listeria, Legionella, Mycoplasma, Mycobacterium tuberculosis, Coxiella burnetii [Q fever], Brucella, Nocardia); Bacterial brainstem encephalitis (Pneumococcus, Salmonella); Parasitic brainstem encephalitis (Taenia solium [cysticercosis], Toxoplasma) ; Viral brainstem encephalitis (HSV1, HSV2, VZV, Echovirus, Coxsackievirus, Other enteroviruses, HIV, Japanese encephalitis virus, West Nile virus, EBV, Adenovirus, CMV, HHV6, Influenza, Rabies virus, Herpes B virus, Poliovirus, JC virus [PML]); Fungal brainstem encephalitis (Aspergillus, Paracoccidioides); 8. Hereditary disorders: Fabry disease; MELAS; MERRF; Metachromatic leukodystrophy; Refsum disease; Wilson's disease; Tay-Sachs disease; 9. Paraneoplastic/paraproteinemic disorders: Paraneoplastic brainstem encephalitis; 10. Traumatic disorders: Traumatic brainstem injury; 11. Iatrogenic disorders: Stereotactic surgery;
Reference:
1. Elan D. Louis, Stephan A. Mayer, Lewis P. Rowland. Merritt’s Neurology, 13 ed. : Wolters Kluwers ; 2016.
2. NeuroAdvise (2018). NeuroAdvise (Version 1.0.0) [Mobile application Software]. Retrieved from http://play.google.com

1 Comment
Morehealthis
13 March, 2020
Behcet s disease with CNS involvement can be divided into two groups: the parenchymal group (80%), which includes hemispheric meningoencephalitis, rhombencephalitis, and involvement of the cranial nerves and spinal cord; and the nonparenchymal type (20%), which includes intracranial venous thrombosis, and arterial occlusion or aneurysm (